
Northeast Georgia Health System (NGHS) saw a surge in COVID-19 cases over the holiday weekend with 181 confirmed cases admitted on Tuesday, December 1, at its hospitals and long-term care facilities combined. The numbers of those needing testing and care are expected to continue rising in the coming days and weeks.
“Both the percentage of tests coming back positive and the number of people who need to be admitted to the hospital have been steadily climbing all month,” said Chief of Medical Staff for Northeast Georgia Medical System Dr. Clifton Hastings. “We’re headed for a new peak and the only question is, how high will this peak be?”
We know people are tired of hearing about wearing masks, washing hands, and watching their distance. Trust me, our nurses, doctors and other staff are tired, too. But those are the only actions that can limit the spread of the virus.
Dwindling hospital bed capacity
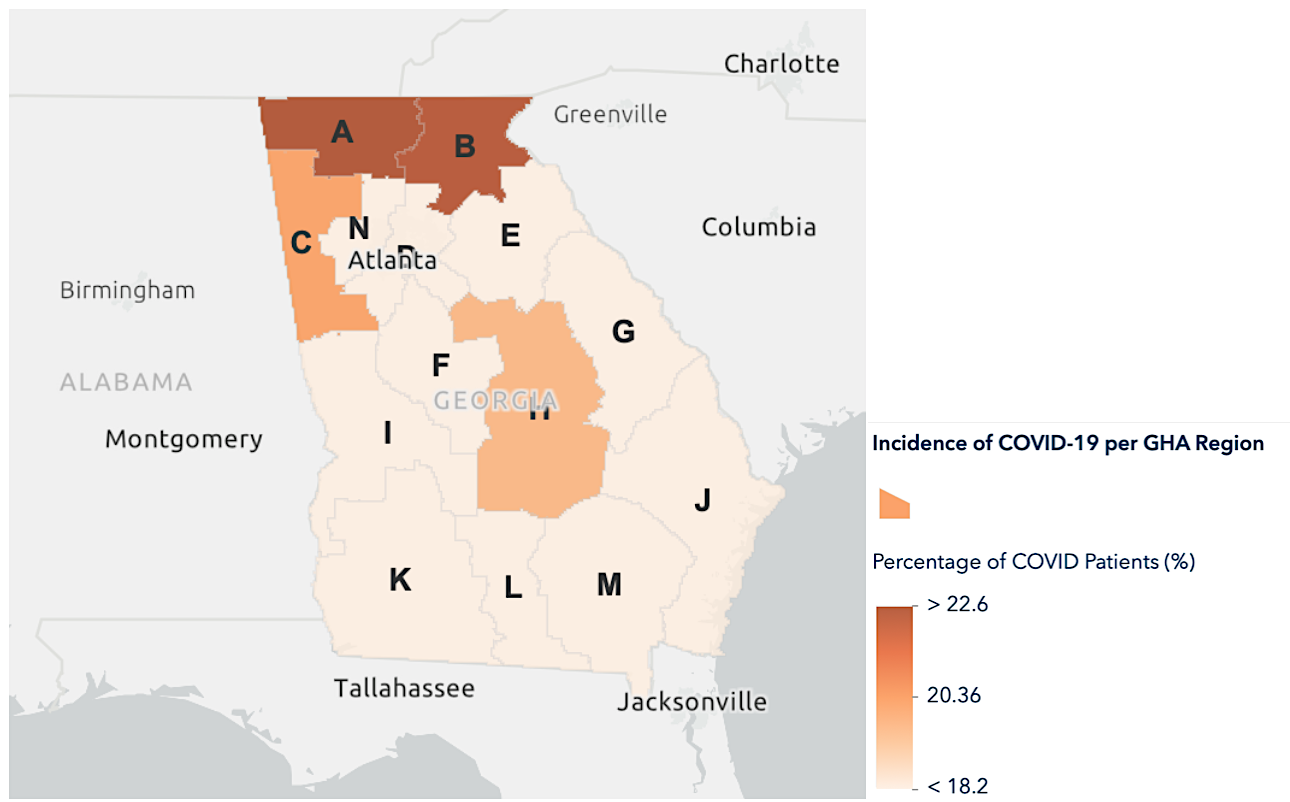
COVID hospitalizations are up across North Georgia and hospital bed capacity is at critical levels. Nearly one-fourth of all patients currently hospitalized in the ten-county Region B area are classified as COVID-19 patients and another 6.8% of the 792 admissions as of December 2 were considered PUI – or patients under investigation for COVID.
Region B includes the counties of Banks, Dawson, Habersham, Hall, Lumpkin, Rabun, Stephens, Towns, Union, and White.
Northeast Georgia Health System’s two largest hospitals in Gainesville and Braselton are nearing full capacity. On December 2, there were 15 general beds and four ICU beds available at Northeast Georgia Medical Center in Gainesville. Braselton had 7 available beds and only one open bed in intensive care. Ventilator use among the system’s four hospitals and two of its long-term care facilities is at 34%.

Habersham Medical Center in Demorest is also experiencing a surge in COVID patients. The hospital is now at 85% of its capacity, according to HMC Vice President of External Affairs Kesha Clinkscale. She says 25% of the patients currently hospitalized in the 53-bed facility are COVID-19 positive.
COVID testing and what you should know
Area health professionals anticipate an increase in the number of people seeking COVID-19 testing in the coming weeks.
“Not only are more people seeking the test because they’re ill, but we expect many will want to get tested so they’ll know whether it’s safe to see family during the holidays,” said Bobby Norris, vice president of operations for Northeast Georgia Physicians Group. “We absolutely want people who think they’re sick to get tested so they can take precautions to protect others, but we also want to avoid premature testing that gives people a false sense of security.”
The entire spirit of the holidays is to think about others first and doing whatever you can to help them, so I hope everyone really takes that to heart and protects the people they love the most.
While they are more readily available now than they were at the onset of the pandemic, testing supplies are still limited, and for most, there is a two- to three-day wait for test results. To help you navigate COVID-19 testing successfully, here are some frequently asked questions:
When and where should I get tested if I have been exposed?
The incubation period for COVID-19 is 14 days, and most patients show symptoms between five and seven days after exposure. It is best to wait 7-10 days after exposure – or earlier if symptoms appear – to be tested. Remember, if you’ve been exposed, you should quarantine following CDC guidelines. To find a testing location near you, visit www.nghs.com/covid-19/testing or contact your local health department.
Am I eligible for the rapid test?
Symptomatic first responders, healthcare workers, and some high-risk patients may get a rapid test depending on availability.
How long will it take to get my results back?
Rapid tests are processed in a matter of hours. All other COVID-19 tests are sent out for processing and returned within two to three business days when the labs can keep up with demand. We have seen surges in testing that caused additional delays at area labs because there were simply too many tests to keep up – and that kind of surge may be possible if the numbers of cases in our community continue to rise.
Should I get a test before seeing family for the holidays?
If you can find a location with enough supplies to accommodate testing for an asymptomatic patient, it’s important to remember:
- The test takes two to three business days to process.
- You may still be exposed to or come down with the virus at any time after testing.
- That’s why it’s still important to take precautions and plan lower risk activities like small events for just your household or virtual gatherings so you can visit with loved ones remotely.
Health officials urge public to help stop the spread
The United States recorded its second-highest single-day COVID-19 death toll on Tuesday with 2,597 new deaths reported. The only day to top that daily total was April 15, when six more deaths were recorded.
According to figures from Johns Hopkins University, more than 270,000 people in the US have died with COVID since January. The country is now averaging over 1,500 deaths a day. While that figure remains lower than the US pandemic peak above 2,240 in late April, it signals an alarming trend that health experts worry will worsen as Americans gather for holiday celebrations and spend more time indoors during the winter months.
“We know people are tired of hearing about wearing masks, washing hands, and watching their distance,” said Dr. Hastings. “Trust me, our nurses, doctors and other staff are tired, too. But those are the only actions that can limit the spread of the virus. The entire spirit of the holidays is to think about others first and doing whatever you can to help them, so I hope everyone really takes that to heart and protects the people they love the most.”
RELATED
Panel: Health care workers, nursing homes first for COVID-19 vaccine







