Nonprofit hospitals in Georgia soon will face tough new financial transparency rules, under a law passed earlier this year by the General Assembly.
The new law will require disclosure of data on executives’ compensation and the financial holdings of hospitals. The state is developing regulations on how it will be implemented, and there is considerable anxiety among Georgia hospital executives as they await the deadlines and rules about the disclosures.
 Representatives of the hospital industry, citing the administrative burden and “vague” terminology in the law, suggested their own set of regulations in July “to implement the law in a fair and reasonable manner.’’
Representatives of the hospital industry, citing the administrative burden and “vague” terminology in the law, suggested their own set of regulations in July “to implement the law in a fair and reasonable manner.’’
But officials under Gov. Brian Kemp say they’re following legislators’ intent and developing pro-consumer rules, not rules favoring hospitals.
“We’re going to work with the hospitals but we will be the drivers of the first draft,’’ said Ryan Loke, chief health care policy adviser to Kemp. “We don’t want the fox guarding the henhouse. We want this consumer-driven.’’
House Bill 321 was approved after much wrangling with hospital industry officials.
It requires nonprofit hospitals to report data including:
- Audited financial information, including charity care provided, on the hospital’s website.
- Financial information about a hospital’s affiliates and subsidiaries.
- All property holdings of the hospital, including the location and size, purchase price and current use.
- Ownership or interest the nonprofit hospital has in any joint venture, partnership, subsidiary, holding company or captive insurance company, and related financial information.
- Any bonded indebtedness, outstanding loans, and bond defaults.
- Salaries and fringe benefits for the 10 highest-paid administrative positions in the hospital.
Failure to comply could bring a cutoff of state health care funding – a devastating penalty for any hospital.
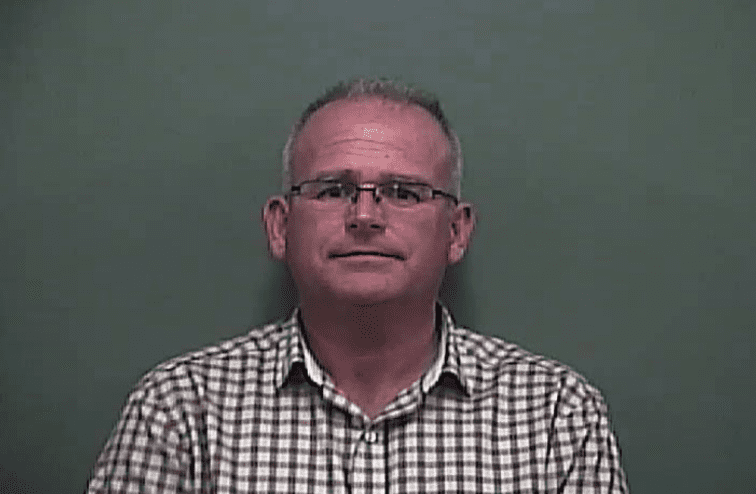
State Rep. Matt Hatchett (R-Dublin), who pushed for these disclosures at the Legislature, told GHN that legislators recognize that “some nonprofit hospitals are hurting and barely surviving.” The communities they serve should know the specifics of the hospitals’ financial distress in order to help them, he said.

“On the other hand, you’ve got nonprofit hospitals that are making lots of money,’’ Hatchett said. “There are those that are amassing huge amounts of cash.’’
Nonprofit hospitals get a tax exemption, he noted, and receive substantial payments from taxpayer-funded programs such as Medicare and Medicaid.
The disclosures could lead to information on hospital overseas accounts. In Massachusetts, 16 hospitals and health systems have more than $1.6 billion in the Cayman Islands and other tax havens, according to a recent report by the Massachusetts Nurses Association.
Regulations on the Georgia law are expected to be released next month. Then there will be a public comment period and potential revisions, which could take another month or so.
Loke acknowledges the statute’s start date of Oct. 1 won’t be met — with the rules still being formulated — and that terms such as “affiliate,’’ “subsidiary’’ and “administrative positions’’ should be more sharply defined.
But he points out that five hospital organizations – Grady Health System, Children’s Healthcare of Atlanta, WellStar Health System, Piedmont Healthcare and Tift Regional Health System – each supported House Bill 321. If those powerhouse systems support the law, Loke says, it should be acceptable to the whole industry.
The Georgia Hospital Association on Tuesday said that nonprofit hospitals don’t oppose transparency. Most of the information required by HB 321 has been publicly available for many years, said Ethan James, a GHA executive.
But the law will add significant expenses for the hospitals, he said. “Especially for some of Georgia’s small, rural hospitals, such unreimbursed costs do exacerbate a sometimes dire financial picture,” he added.
 “In order to best utilize the collective experience and knowledge of the hospital industry and serve as a partner and resource for state policymakers, the Georgia Hospital Association offered initial comments to DCH [the state’s Department of Community Health] early this summer regarding the development of the pending rules and regulations,’’ James said. “We look forward to working in concert and receiving additional guidance from the Department of Community Health and Governor Kemp’s staff.”
“In order to best utilize the collective experience and knowledge of the hospital industry and serve as a partner and resource for state policymakers, the Georgia Hospital Association offered initial comments to DCH [the state’s Department of Community Health] early this summer regarding the development of the pending rules and regulations,’’ James said. “We look forward to working in concert and receiving additional guidance from the Department of Community Health and Governor Kemp’s staff.”
Chris Kane, senior vice president of consulting firm Nagle & Associates, said the law “represents progress in the quest for transparency in health care.’’
“For hospitals and health systems, compliance will be tedious because some reporting requirements are new and others encompass reformatting existing information.’’
Kane said transparency “is an imperative for a sector that has largely operated under the radar under the premise that a nonprofit organization will pursue activities consistent with societal priorities. Yet the consolidation of health care and growth and demand has created behemoths.’’
Some of the law’s terms and requirements are either ambiguous or need tweaking, Kane added.
Hatchett said he could live with some changes. For instance, if a hospital doesn’t have a website, the financial data could be posted on the website of its parent system.
And if a small hospital doesn’t have 10 administrative positions that offer more than $100,000 a year in compensation, the smaller salaries could be omitted, he said.
Nevertheless, Hatchett said, public scrutiny of the financials could lead indirectly to hospitals lowering health care costs, which consume a large part of families’ budgets.
“People have the right to know where public money is going,” he said.