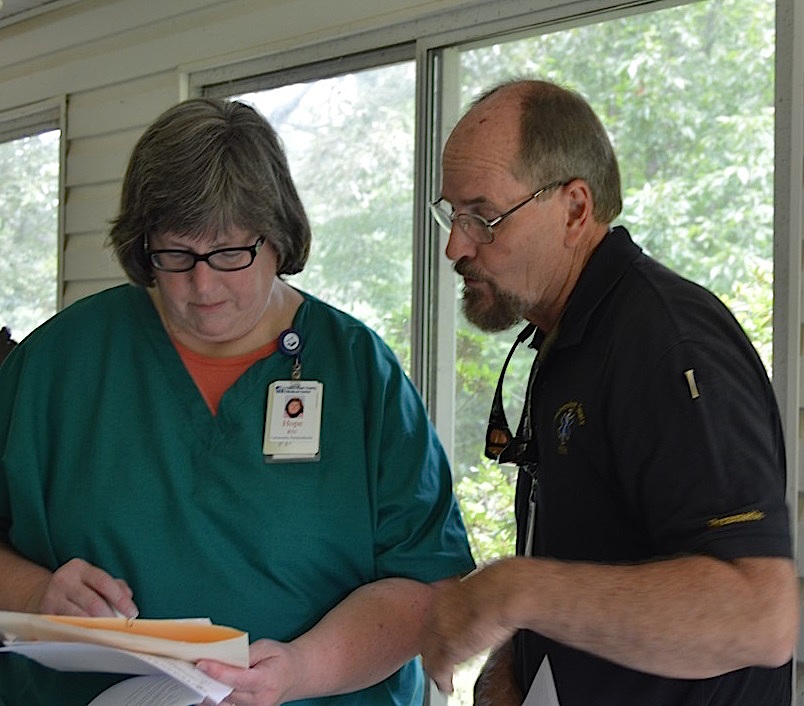
As a Paramedic, Jim Wood has treated thousands of patients during his forty-year career with Habersham EMS. Jim’s job has always been to transport patients to an Emergency Room (ER). But, today his job has taken a different twist and his new focus is to keep patients at home and out of the ER.
Along with Hope Adams, a Registered Nurse at Habersham Medical Center, Jim is part of a new program called Community Paramedicine. Their primary role is to provide home visits to the underserved who have chronic illnesses such as congestive heart failure, mental disorders, lung disease, and diabetes to help them comply with their prescribed treatment plans.
Many of the patients they treat are “frequent filers” or regulars in the Habersham Medical Center ER or have been hospitalized repeatedly for the same chronic condition because of noncompliance. Thus, the program is also a hands-on approach to reduce misuse of valuable and expensive emergency room resources and reduce unnecessary hospital readmissions. “Most rural hospitals like Habersham Medical Center are losing millions of dollars from bad debt and charity care from misuse of the ER or readmits that hospitals are financially penalized for,” Jim says. “So, our focus is on keeping these patients well.”
Currently, there are 27 patients enrolled in the Community Paramedicine program. “When we first pulled the list of frequent users, it was overwhelming,” adds Jim. “We had to narrow down the list considerably. Program participation is by selection only, and our current patients range in age from 30-93, and we try to visit each patient at least once a week.”
At each visit, Hope and Jim assess the patients’ vital signs and provide preventative care. According to Hope, “We also assess their home environment to see if they have any fall hazards; check to see if they have heat and air; inspect their food supply and help them comply with discharge instructions and follow-up appointments. We really try to get to know each one of our patients. We’ve become like family. We know their life stories and ask lots of questions. We are finding that the best way to “treat” most of these patients is to take care of the underlying social needs or financial barriers to taking care of themselves.”
Many do not have transportation or cannot afford public transportation and often call an ambulance to transport them to the ER for mostly non-emergent conditions. “One of our patients used to call EMS every morning! Now, we drop by to visit her in the comfort of her own home at least twice a week and she hasn’t had to be transported in a while. She loves our visits and is always excited to see Jim. Older women just love Jim,” laughs Hope.
Most have been very receptive to the home visits. “One sweet lady had to warm up to me but now she will welcome me at the door with a big hug,” Hope adds. “During a recent visit, she talked for more than an hour! Sadly, most of our patients are lonely and just need someone to show them they care. A little attention goes a long way.”
Hope and Jim also work closely with many local healthcare and social service organizations like free clinics and food banks. “Many do not know what community resources are available to them, don’t have access, or can’t complete the paperwork,” Jim says. “It is overwhelming to them. And, many of them just need someone to help them wade through the paperwork needed to apply for financial assistance.”
“Today, we dropped in on an elderly man who was very short on food and had a water leak that needed immediate attention, so we are in the process of trying to contact his landlord. We also had to pick up a prescription for a patient at the pharmacy because she had no transportation. And, we helped a family get $50 to turn their power back on, and we are working with an elderly gentleman to get him moved into government housing.”
Hope adds, “A diabetic patient we saw today had a blood sugar level over 400 during our first home visit. Today, her level was down to 100; a significant improvement! All she needed was regular doctor’s appointments and education on diabetes management.”
Another patient on the schedule today needed help organizing her medications. When asked if she was pleased with the Community Paramedicine program, she quickly exclaimed, “Lord, yes! I love them!” I am so forgetful. I could not keep track of my medications and when filling up my pillbox, I would always end up with extra pills or would forget to take them.”
Jim is quick to point out, “These are not people who just refuse or cannot work; many of these are retired senior citizens who can’t live on their meager social security checks. It’s sad when a Korean War Veteran has to choose between buying food or his medications,” Jim adds. “Yes, people could argue that most people need to make better life choices. Yes, some are there by choice, but most are dealing with the cards they have been dealt. We don’t judge, we treat.”
“Our goal is to graduate the patients after a few visits,” says Hope. “We provide them with resources and education and then once they can take control of their own health, we will release them from the program and select additional patients.”
The new Community Paramedicine home visits began in April 2017 and it is being funded by the $1 million grant Habersham Medical Center received from the Georgia Rural Hospital Stabilization Committee. In addition to Habersham Medical Center’s other new business models to reduce misuse of the ER – the new ER screening process and extending Prime Care’s hours of operation to seven days a week – the Community Paramedicine program will be evaluated for its effectiveness and may be used by other rural hospitals across the state to help improve their financial hardships.
“There is no way to charge for this program,” says Tyler Williams, HMC Project Manager. “While hospitals across the nation have similar programs, this is still an emerging field. Maybe one day we can receive additional government funding for this program. But, right now, if we can keep these patients out of the ER or from calling an ambulance for a non-emergent issue, then we are saving lots of money. So, in a way this program more than pays for itself.”
Nevertheless, to Hope and Jim, the program is a win-win. “It’s a very humbling experience,” says Hope. “We’ve seen a lot in a few short weeks. The needs are heartbreaking, but at each visit, we see improvement in these patients’ health and quality of life, and we call that a major success.”