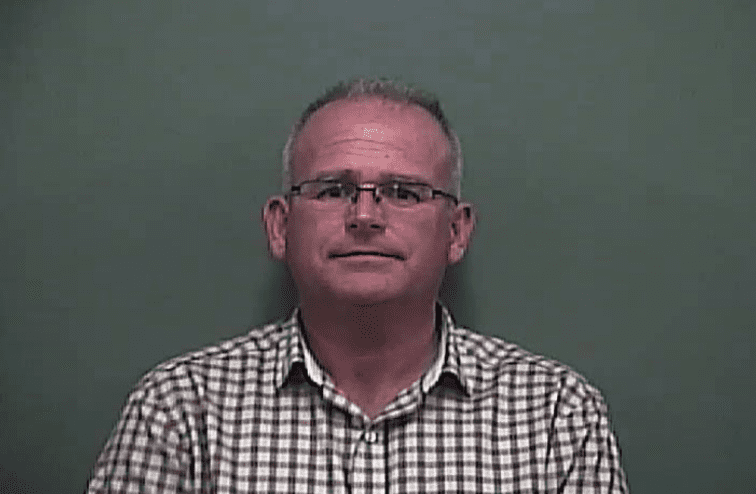
Fabian Kausche doesn’t plan on getting a tattoo any time soon, and without much hair, a visit to the barbershop isn’t a priority either. Even though personally, he may be safe to do so.
In mid-March, Kausche tested positive for COVID-19, the disease caused by the novel coronavirus. He was ill for three weeks, but the 58-year old veterinary scientist from Johns Creek is now “one hundred percent recovered.”
As a COVID survivor, Kausche probably has a certain level of protection against the virus. But he won’t know for sure until researchers learn more about how immunity against the new virus really works.

Kausche
The answer for him, as for tens of thousands of recovered patients and others infected without symptoms, lies in antibodies, proteins in the blood produced by the body while fighting off a virus. For many virus infections, the presence of antibodies indicates a person is at a lower risk of getting re-infected for a period of time.
Around the world, research institutions and private companies are ramping up development, production and rollout of antibody, or serological, tests.
But so far, antibody testing in the U.S. is as uncoordinated and non-transparent as the earlier testing for active COVID-19 infections.
“It looks like chaos, and it is chaos,” says Bill Custer, a health economist at Georgia State University. The testing situation shows how unprepared the country was for the pandemic, he adds. “We are still playing catch-up.”
Antibody testing serves a threefold purpose in the next chapter of the coronavirus response.
- It’s an important public health tool to get a better overview of how the novel coronavirus has spread in communities, and a guide to safely opening up the economy.
- It is at the core of research efforts to better understand the disease, find effective treatments and eventually develop a vaccine for the virus.
- One of the more promising investigative treatments for COVID-19, convalescent plasma, is based on the power of antibodies.
The state of Georgia is following in the footsteps of New York by conducting an antibody testing survey to get a better idea of how many people have been exposed and have developed antibodies to SARS-CoV2, the virus that causes COVID-19. For the study, the Georgia Department of Public Health has partnered with the CDC and the boards of health of Fulton and DeKalb counties. Until May 4, teams of public health workers will visit randomly selected homes in different areas of Fulton and DeKalb and ask residents to provide blood samples.
The preliminary results of a similar study in New York indicated that 15 percent of people in the state had antibodies against the virus, and the figure was 21 percent in New York City, which has become the epicenter of the crisis in the United States.
The study confirmed experts’ suspicion that many more people may have been infected with the virus than those who tested positive for active COVID-19.
According to the FDA, close to 200 companies and laboratories have already signed up to offer antibody tests in the U.S. But so far, only seven tests have received fast-track approval by the agency.
 The FDA in March eased its rules after the agency had initially been criticized for slowing down authorization of diagnostic tests for active COVID infection. The move resulted in a barrage of antibody tests flooding the market without formal approval. Companies still have to do their own validation of their tests and notify the FDA. They are also required to label their products as non-FDA-approved.
The FDA in March eased its rules after the agency had initially been criticized for slowing down authorization of diagnostic tests for active COVID infection. The move resulted in a barrage of antibody tests flooding the market without formal approval. Companies still have to do their own validation of their tests and notify the FDA. They are also required to label their products as non-FDA-approved.
The majority are rapid tests, which typically use a finger-stick amount of blood on a test strip and yield a “yes or no” result, indicating whether or not the patient has antibodies. Others are quantitative tests that provide a more detailed evaluation of the types and levels of antibodies the immune system has produced after fighting off COVID-19.
The tests, many of which are manufactured in China, are sold to hospitals, urgent care clinics, doctors’ offices, first responders and private businesses. There are some home antibody test kits available online, but those are not approved by the FDA.
The rationale behind the FDA’s decision to loosen its restrictions was “to encourage more tests to get on the market,” says Custer, and to get large portions of the population tested faster.
The American Medical Association, in a letter to the U.S. Department of Health and Human Service, expressed concern about the current state of COVID-19 antibody testing. The AMA asked for stronger federal guidance “to ensure tests offered to the public are accurate and used appropriately.”
The Association of Public Health Laboratories has warned that many of the new tests are unreliable and widely inaccurate. “Right now, it’s a Wild West show out there,” APHL chief program officer Eric Blank told the Associated Press. His group represents more than 120 state and local public health labs.
For example, a test may generate a false positive, telling people they have antibodies and therefore suggesting they have immunity, when in fact they don’t. “That’s a real danger and concern,” says Custer. “And if there’s a lot of uncertainty, it’s going to be very difficult to restart the economy.”
Trying to answer a lot of questions
In addition to being an important public health tool, antibody testing is also key to studying the novel virus, says Dr. Aneesh Mehta, a professor of infectious diseases at Emory University’s School of Medicine.
“And, we can also use antibodies to find a therapy and help target a vaccine,” he says

The Kausches
Emory has developed an antibody test to better understand the immunity response in people who had previously been infected with COVID-19. Currently, the test is only available to Emory Healthcare workers, as well as certain patient groups in the Emory system.

The Kausche antibody test results
Emory is testing at a rate of 300 people per day but plans to quickly scale up. By mid-June, researchers hope to test 5,000 people per day and eventually offer the test to the wider community.
Emory’s antibody test is performed as a standard blood test, requiring the drawing of one vial of blood. Mehta says the test is “very sensitive and very specific” to the proteins that can only be found on SARS-CoV2. “Our test will not cross-react with other coronaviruses,” Mehta says.
Some of the standard tests have been criticized for responding to a broader range of coronavirus antibodies. There are several varieties of coronaviruses, some of which cause the common cold and some that are responsible for more severe infections like SARS and MERS.
Most experts suggest recovered COVID patients will have a certain level of immunity for at least a couple of months, but there’s no clear evidence yet. Last week, the World Health Organization (WHO) warned that there is no guarantee of immunity for COVID-19 survivors.
That’s why the Emory researchers want to learn more about how immunity works in those recovered from COVID. What type of antibodies are they producing? Do they have what virologists call neutralizing antibodies that are particularly powerful in helping the immune system kill off the virus? If antibodies protect against the novel coronavirus, how strong is the immunity, and how long does it last?
Mehta says he and his colleagues also want to find out “if there are differences in protection between survivors who had no symptoms or mild symptoms and others who experienced moderate or severe symptoms.”
If a correlation exists between the severity of the disease and the strength of the protection, Fabian Kausche should have solid immunity.
On March 15, he developed a dry cough and a fever with chills and night sweats. “And a weakness so extreme that I wasn’t able to get out of bed for more than two or three hours at a time,” he recalls.
Kausche, who is German-born and married to state Rep. Angelika Kausche (D-Johns Creek), was lucky that his primary care doctor happened to have a diagnostic nasal swab test available, so he got tested and was confirmed positive for COVID-19 within a few days.
For the following three weeks his condition plateaued. “I was feeling awful, but stable awful,” he says. “It just wouldn’t change.” The scariest part was not knowing what to expect, says Kausche, an avid cyclist who typically rides 40 to 50 miles each day.
After 17 days, he finally started to feel better. A week after he became ill, Angelika got sick, too, but her symptoms were mild. She didn’t get tested and recovered within a few days.
After he was well again, Fabian Kausche felt the need to spread the word among friends, neighbors and co-workers that “this virus is nothing to be nonchalant about. This is serious.”
He told his primary care doctor, who is associated with the CDC, as well as other physician friends, that he would be happy to be part of any clinical trial that would help find a cure or a protection for the disease.
He and his wife took a rapid antibody test at their doctor’s office, and it confirmed that they both had developed antibodies to the new coronavirus.

Rep. Kausche
The couple continue to wear masks when they go to the grocery store – “just to send a message that this is the responsible thing to do,” says Angelika Kausche. After all, she adds, strangers who see them can’t know that they have recovered from the disease and probably can’t spread the virus.
With their presumed immunity as a protection for themselves and others, the Kausches would also like to help out in the community, in hospitals, nursing homes or assisted living facilities. But with the unknowns about how immunity works for the new virus, Fabian Kausche says it’s not safe yet to resume normal life.
“As a scientist, as a citizen and as a potential volunteer, I would love to have the data that tell us how immune somebody who has recovered from COVID-19 really is, and how long immunity lasts,” he adds.
Survivor wants to ‘give back’
Dr. Alan Kozarsky also wants to make sure something good comes out of the illness he has beaten. The 67-year-old Atlanta ophthalmologist and flight doctor started to develop a dry cough and a mild fever on March 9 while on a mission trip to Honduras. Kozarsky, who is slim, wiry and has no medical risk factors, immediately returned home, isolated himself and contacted the patients and colleagues he had been in touch with the week before he became symptomatic. He got tested a few days later, and by the time his result came back positive he had almost recovered.
“I felt so lucky to have gotten off so easily from this disease,” Kozarsky says. “The questions were going through my head: How can I help? How can I give back?”
He heard anecdotal evidence that convalescent plasma, rich in antibodies of COVID survivors, has helped some severely ill patients. Plasma is a straw-colored liquid component of blood, and convalescent plasma is the type that can be collected from patients who have recovered from an infection. It’s one of the treatments that’s being investigated for the novel coronavirus disease.

Kozarsky
“This is not a new method,” Kozarsky explains. Doctors have used convalescent plasma for over 100 years, trying to help patients fight off the Spanish flu, polio, measles or more recently, Ebola, SARS, MERS, and the 2009 H1N1 pandemic, also known as the Swine Flu.
The physician signed up with Atlanta Blood Services, an affiliate of Northside Hospital’s Blood and Marrow Transplant Group that collects donor plasma and then administers the fluid to critically ill COVID patients hospitalized at Northside. Other health systems in the state are running similar programs, including Floyd Medical Center in Rome and Memorial Health in Savannah. Hospitals in the Wellstar system are part of a collaboration between the Mayo Clinic, the FDA, the American Red Cross and more than 40 hospitals across the nation.
It’s his second time giving plasma in the past two weeks, Kozarsky says over the phone, as he sits in a room with other donors at Atlanta Blood Services. During the 30-minute procedure called plasmapheresis, his blood is drawn from a vein in his arm, and a special machine then separates the red blood cells from the plasma. The red blood cells are then returned to his body while the plasma is collected in a small, clear plastic bag.
Kozarsky says he wants to donate convalescent plasma for as long as he can, but a lot depends on what antibody research will come up with, and how long the presumed immunity lasts.
Currently, only individuals who have a documented diagnosis of COVID-19 and have fully recovered from the disease for at least 14 days are eligible to donate plasma. But as the need for the investigational treatment increases over the next couple of weeks, it may be necessary to expand the corps of plasma donors to those who have not been tested for an active infection but have developed antibodies against the virus.
But as long as there is a flood of unregulated antibody tests with unknown failure rates, “this could potentially be very dangerous,” Kozarsky says, adding that this is another reason “why it’s so extremely important to develop highly accurate antibody tests.”
Kozarsky’s advice to COVID survivors who want to help is to contact a major health care system in their area or ask their primary care doctor for guidance. Also, the American Red Cross is seeking recovered COVID patients to sign up for plasma donations. Fabian Kausche has already submitted his information to the program.
Emory’s Dr. Mehta also recommends that volunteers get in touch with The Hope Clinic at Emory, which is recruiting COVID survivors to study their antibodies for various clinical trials.

Mehta Photo credit: Emory University
On the research side, Mehta says it’s critically important that as many agencies, universities, hospitals, laboratories and companies around the world develop, study and evaluate different antibody tests. “There will be a lot of tests, and they may add to some confusion early on,” he admits, adding that the process is key to making sure “that in the end, we will find the test that works best.”
Fabian Kausche and Alan Kozarsky don’t want their fellow COVID survivors — those with a documented diagnosis and those without one — to be discouraged by the current chaos of antibody testing, and the competing trials, studies and surveys.
As people who’ve had COVID-19 and recovered from it, “we’re specially positioned to help,” says Kozarsky, “and we should take advantage of every opportunity to do so.”
Katja Ridderbusch is an Atlanta-based journalist who reports for news organizations in the U.S. and her native Germany. Her stories have appeared in Kaiser Health News, U.S. News & World Report, and several NPR affiliates.