ATLANTA — When Destiny heard screams, she raced to a hospital room where she saw a patient assaulting a care technician. As a charge nurse at Northeast Georgia Health System, she was trained to de-escalate violent situations.
But that day in spring 2021, as Destiny intervened, for several minutes, the patient punched, kicked, and bit her. And by the time a team of security guards and other nurses could free her, the patient had ripped out chunks of Destiny’s hair.
“We are not protected on our floors,” she said as she recapped the story during testimony later that year to the Georgia Senate Study Committee on Violence Against Healthcare Workers. Destiny used only her first name at the hearing for fear of retaliation for speaking out against the patient who assaulted her.
In May, Republican Gov. Brian Kemp signed a law that boosts criminal penalties for assaults against hospital workers and allows healthcare facilities in the state to create independent police forces. The law is a response to that testimony as well as hospital lobbying and data documenting a rise in violence against healthcare workers. In enacting the law, Georgia joined other states attempting to reverse a rise in violence over the last several years through stiffer criminal penalties and enhanced law enforcement.
Nearly 40 states have laws that establish or increase penalties for assaults on healthcare workers, according to the American Nurses Association. And lawmakers in 29 states have approved or are working on similar laws, as well as ones that allow the creation of hospital police forces. Members of those forces can carry firearms and make arrests. In addition, they have higher training requirements than noncertified officers, such as security guards, according to the International Association for Healthcare Security and Safety.
Groups representing nurses and hospitals argue that such laws address the daily reality of aggressive or agitated patients who sometimes become violent. Still, such interventions are relatively new. Critics worry that establishing hospital police forces will escalate violence in healthcare settings and could have downstream effects.
“I worry about all the reasons patients have not to trust me and trust the health care system,” said Elinore Kaufman, a trauma surgeon at the University of Pennsylvania.
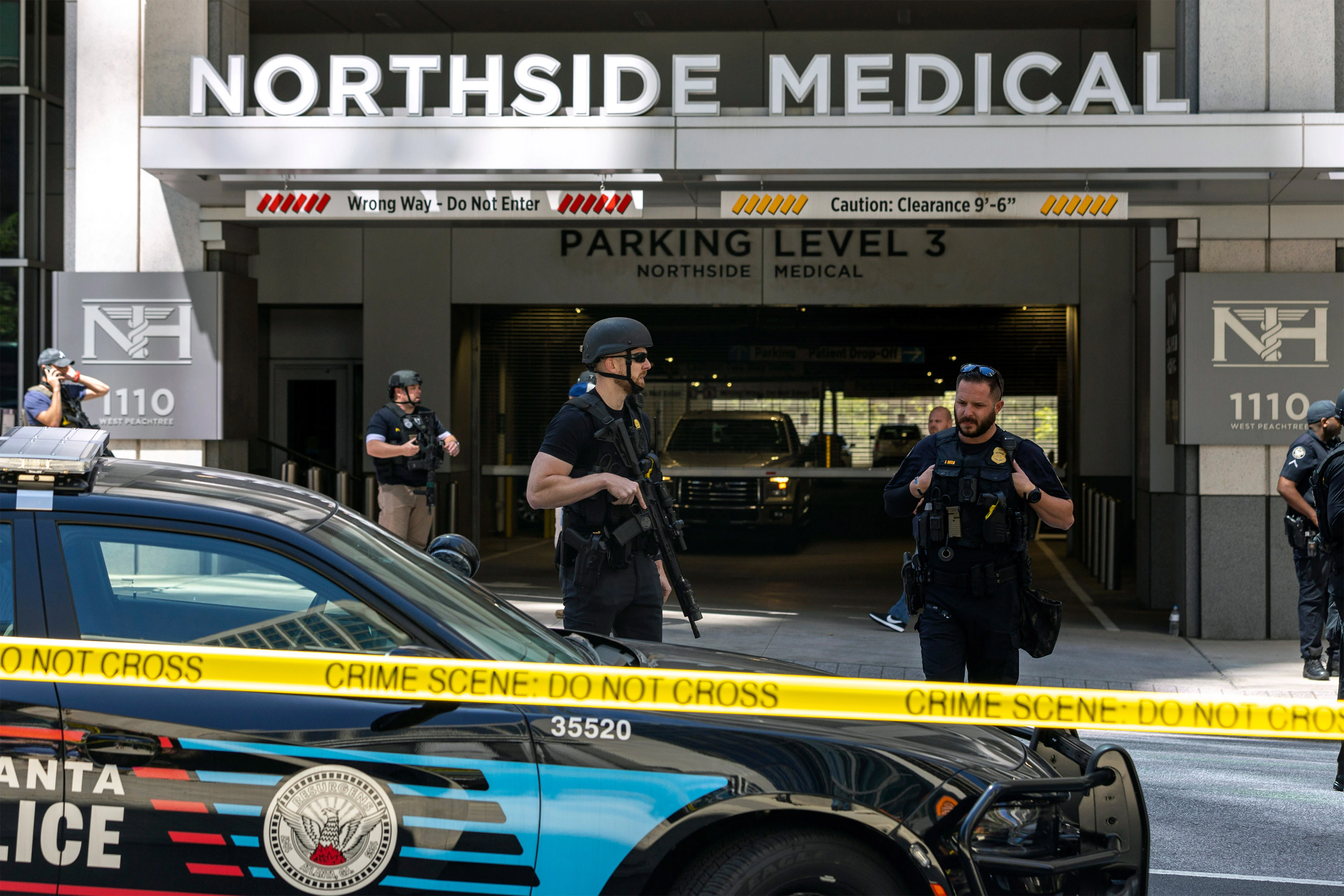
Healthcare workers are five times as likely to experience violence as employees in other industries, according to federal data. The day after Kemp signed the Safer Hospitals Act into law, a person opened fire in a midtown Atlanta medical office, killing one woman and injuring four others, including workers at the medical practice.
Verbal and physical threats, which increased during the pandemic, are exacerbating a dire nursing shortage, said Matt Caseman, CEO of the Georgia Nurses Association. Destiny testified that one of her co-workers left nursing after the 2021 assault, in which the patient smashed the care technician’s face into a wall and the floor. Destiny also suffered from post-concussion headaches for months, she said.
The Centers for Medicare & Medicaid Services noted the alarming rise of violence in healthcare settings last November. The federal agency recommended hospitals implement a patient risk assessment strategy, increase staffing levels, and improve training and education for staffers. There was no mention of boosting law enforcement presence.
Health centers say they are better able to retain workers and improve patient care when they can reduce the number of violent incidents, said Mike Hodges, secretary of the Georgia chapter of the International Association for Healthcare Security and Safety. State laws governing how hospitals can respond to violence vary.
In Georgia, the new law boosts criminal penalties for aggravated assaults against all healthcare workers on a hospital campus, not just those in emergency rooms, which were already regulated. And hospitals can now establish law enforcement offices like those on university campuses. The officers must be certified by the Georgia Peace Officer Standards and Training Council and maintain law enforcement records that can be made public.
Having a dedicated police force helps hospitals better train officers to work in a healthcare setting, said Republican State Rep. Matt Reeves, who co-sponsored the Georgia bill. Officers can get to know staff members and regular patients, as well as the layout and protocols of hospital campuses. “If you have a specialized police department, they are more in tune with the needs of the facility,” he said.
That’s the case at Atrium Health Navicent, which operates hospitals across central Georgia, said Delvecchio Finley, its president. The health system was one of a handful to staff certified law enforcement before the new law.
Atrium Health recruits officers who reflect the diversity of the community, conducts training to counteract implicit biases, and holds debriefings after any incidents, Finley said. Officers are trained to react when someone becomes violent at one of the facilities.
“The biggest thing for us to convey to officers is that they are in the setting where we provide a safe environment where we care for anyone,” he said.
Unlike other businesses, hospitals can’t merely throw out patients who misbehave, said Terri Sullivan, an emergency nurse in Atlanta. A patient once punched her in the chest, fracturing two ribs, before running out of the room and trying to punch his physician. Sullivan said that, in her experience, the presence of hospital security can prevent patients from acting out.
Still, little data exists on whether such forces are effective at preventing hospital violence. Ji Seon Song, a University of California-Irvine law professor who studies policing in healthcare settings, worries about the “unintended consequences” of legislation that boosts the presence of law enforcement in places people receive medical care.
“You can see where there might be a lot of problems,” she said, “especially if the patient is African American, undocumented, Latino — something that makes them prone to being criminalized.”
A ProPublica investigation found Cleveland Clinic’s private police force disproportionately charges and cites Black people. And in March, a video emerged showing police and hospital staff members in Virginia holding down a patient who was experiencing a mental health crisis, leading to his death. In 23% of emergency department shootings from 2000 to 2011, the perpetrator took a gun from a security officer, according to a Johns Hopkins University study. The CMS memo noted several hospital incidents involving police, in which the agency cited the facility for failing to provide a safe environment.
The Georgia law doesn’t require hospital police officers to arrest patients with outstanding warrants for offenses that occurred off a hospital campus, such as violating probation. But it doesn’t limit those powers either, said Mazie Lynn Guertin, executive director of the Georgia Association of Criminal Defense Lawyers.
“Unless discretion is limited, it will be exercised at some point, by someone,” she said.
Law enforcement should always be the last resort, argued Kaufman, the trauma surgeon. While the threat of violence is concerning, hospitals can spend more on healthcare staffing, boost overall training, and teach de-escalation skills.
“Our primary lens shouldn’t be that our patients are a danger to us,” she said. “It’s a harmful lens and a racist one. We should develop safe and healthy workplaces through other ways.”
____________
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.







