(GA Recorder) — Hundreds of thousands of Georgians who have had health insurance through Medicaid during the pandemic could begin to lose their coverage this coming spring under the proposed federal spending bill unveiled this week.
The congressional proposal would end the pandemic-era rule requiring states to continue covering Medicaid enrollees even if they no longer qualify under a state’s eligibility rules. The requirement was packed into federal coronavirus legislation passed in March 2020.
Under the terms in the $1.7 trillion spending package, millions of people could lose coverage nationally – including about 545,000 Georgians, according to one state estimate – under a process that could start as soon as April 1 if Congress passes the federal spending bill.
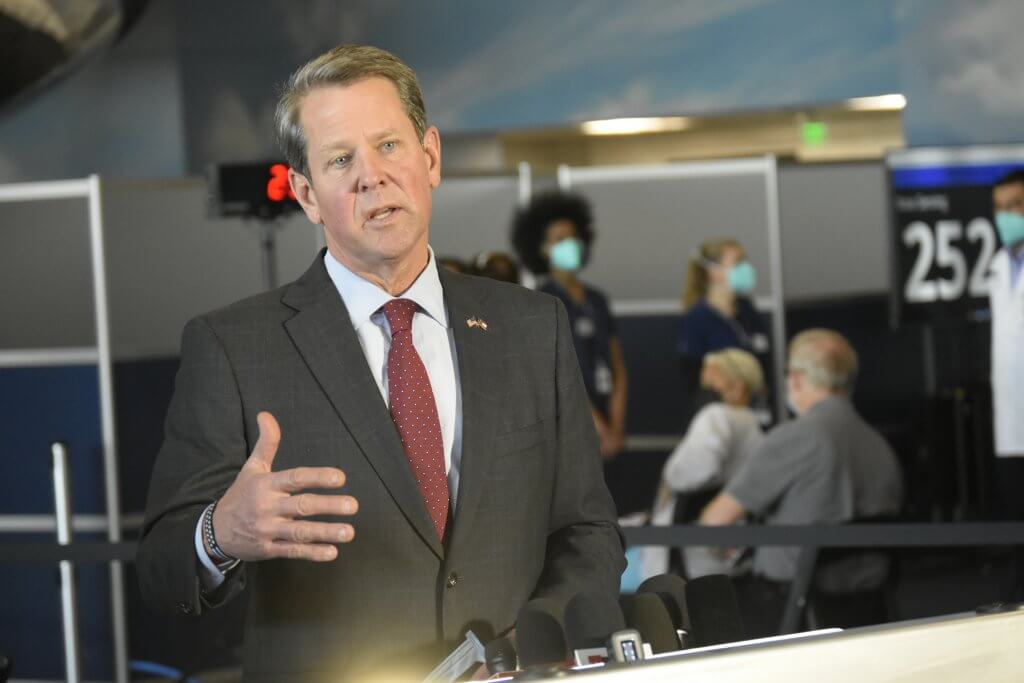
A group of Republican governors, including Georgia Gov. Brian Kemp, sent President Joe Biden a letterthis week asking him not to renew the public health emergency declaration beyond April so states could start whittling down their inflated Medicaid rolls, citing the costs.
The governors’ plea was made even as states continue to wrestle with a “tripledemic” of rising COVID-19, flu and RSV cases that threaten to strain their hospitals this winter.
“While the virus will be with us for some time, the emergency phase of the pandemic is behind us,” the 25 governors wrote in a Dec. 19 letter to Biden. “We have come so far since the beginning of the pandemic – we now have the tools and information necessary to help protect our communities from COVID-19.”
The emergency declaration is set to expire Jan. 15, but the Biden administration is expected to extend it again, continuing it through at least April. But the proposed spending bill would untether the so-called Medicaid unwinding process from the federal emergency declaration.
In Georgia, Medicaid enrollment has grown to about 2.6 million people, up from about 1.8 million before the pandemic.
That increase has come with extra federal funding that helped state budget writers navigate the public health crisis, delivering Georgia about $2.2 billion in fiscal relief – or more than twice the amount the state spent on additional enrollees, according to an analysis from the Kaiser Family Foundation.
The state closed out the last fiscal year with a $6.6 billion surplus, and revenues for the first five months of the new budget year were up 6.2% – or $741.7 million – above this time last year.
But even with the federal boost, GOP leaders argue the rule has cost states “hundreds of millions of dollars,” the letter said.
“The PHE is negatively affecting states, primarily by artificially growing our population covered under Medicaid (both traditional and expanded populations), regardless of whether individuals continue to be eligible under the program,” according to the letter.
There won’t be a clear picture of the cost until states are able to go through the process of identifying those who are no longer eligible for coverage because, for example, they have aged out of the program or their income level has changed, said Kemp’s spokesman, Andrew Isenhour.
All told, though, the state has spent about $37.5 billion on Medicaid enrollee benefits since the beginning of the pandemic, Isenhour said.
Under the proposed omnibus, the enhanced federal match for states would be phased out over the next year, and it would also require a year of continuous coverage for children in low-income households.
‘A life preserver’
Health care advocates are urging Georgia officials to move cautiously as this key pandemic-era rule, which has guaranteed health care coverage for a wide swath of Georgians, comes to an end.
The policy has been a success, says Leah Chan, senior health analyst with the Georgia Budget and Policy Institute.
“During a time of both health and economic uncertainty, this policy kept almost three million Georgians connected to affordable health coverage and brought fiscal relief to our state,” Chan said.
It’s important for the feds to establish a date for the Medicaid unwinding to begin – as has been proposed in the omnibus – so state officials, Medicaid managed care organizations, community leaders and others can prepare, she said.
“But we cannot go back to our pre-pandemic status quo where Georgia had one of the highest rates of uninsurance in the country,” Chan said. “We have a unique opportunity during the Medicaid unwinding planning process to adapt what worked well and build upon the success of this policy so that Georgia’s families stay covered.”
Laura Colbert, executive director of Georgians for a Healthy Future, a consumer advocacy nonprofit, called Medicaid “a life preserver” for people and states during the pandemic.
“Its continuous coverage protections have enabled Georgia children, expecting and new parents, and others to get covered, stay covered, and affordably access health services in the midst of a very unpredictable pandemic,” she said.
Federal and state investments in Medicaid should match the reality on the ground, Colbert said, pointing to the triple epidemic and low rates of vaccination for COVID-19 and the flu.
“State and federal leaders should consider these ongoing challenges and adjust Medicaid funding and protections as appropriate,” Colbert said. “As a state with among the highest uninsured rates for children and adults, I would caution against rushing towards the end of the PHE, which will end Medicaid’s continuous coverage protections.
“As a result, we expect between 245,000 to 545,000 Georgians to become temporarily or long-term uninsured. More than half of the newly uninsured will be kids,” she added.
In the meantime, state agencies have been encouraging Georgians with Medicaid coverage to update their contact information through their Gateway account.







