From waivers to toxic pollution to disease outbreaks, Georgia experienced an eventful year in health care. Here is our list of the Top 10 health care stories in 2019.
1. Gov. Brian Kemp unveiled proposals to offer more people Medicaid coverage and improve private insurance.
Just as 2019 ended, the Kemp administration finalized its health care proposals, which will require approval by the feds. One waiver request would add more low-income Georgians to Medicaid. Democrats repeatedly emphasized that the plan’s eligibility requirements would cover far fewer people than Medicaid expansion under the Affordable Care Act. But Kemp and his fellow Republicans who control state government made clear that their opposition to Medicaid expansion had not changed. A second waiver proposal calls for a ‘‘reinsurance’’ program, plus a plan to replace the state’s current healthcare.gov website procedure with what officials say would be a more consumer-friendly enrollment process.

2. Ethylene oxide — the invisible danger. It’s likely that most Georgians had never heard of ethylene oxide until 2019. Then, a July report by WebMD and Georgia Health News revealed that Georgia has three census tracts with elevated risks of cancer from air pollution, largely due to this gas. Ethylene oxide, which is used to sterilize medical equipment, quickly became a contentious topic in Georgia. The risk areas are near sterilization plants that use the gas – news that led to community protests and more government scrutiny. One sterilization plant, Sterigenics in Cobb County, was closed until it could meet county safety standards, and it remains closed as of year’s end. Another facility, the BD plant in Covington, reported in December that its nearby warehouse had high emissions of ethylene oxide.
3. Hundreds of abuse and neglect violations were reported at senior care facilities. AJC investigative reporters studied thousands of documents regarding assisting living communities and personal care homes and identified more than 600 allegations of neglect and 90 of abuse. Gov. Kemp’s office and several lawmakers said the series revealed problems that must be addressed in these senior facilities.
4. Flooding shut down more than 200 beds at Grady Memorial Hospital. It was not an epic storm but a burst pipe that unleashed waves of water in parts of the Atlanta safety-net hospital in December, but the damage to property and equipment was severe. It was so extensive that Grady’s famously busy emergency room was briefly accepting only walk-in patients. The crisis rippled through much of metro Atlanta, as other hospitals mobilized to take in patients that Grady could not handle. Some of the damage at Grady will take months to fix, and a mobile hospital has arrived on the grounds to serve more patients.
5. Public Health officials responded to measles, Legionnaires’ disease, hepatitis A, and vaping-related illnesses. No cases of measles had been reported in Georgia for three years, until 2019, when the state had 18 such illnesses, including 11 in Cobb County, all among unvaccinated individuals. An Atlanta hotel was hit by at least 13 confirmed cases of Legionnaires’ disease, including one that was fatal.Hepatitis A remained a scourge in the northwest part of the state, as well as other areas, with hundreds of cases reported since 2018. And Georgia, like other states, experienced a spurt of vaping-related lung illnesses, including five deaths here.
6. An Atlanta neighborhood was found contaminated with lead. An Emory research team discovered lead contamination in the soil in a neighborhood in west Atlanta. Those findings led to an EPA investigation, which determined that more than half of the properties tested in that area had high levels of the toxic metal, a situation that is particularly dangerous to children. The federal agency promised to fix those properties, while people in neighboring communities wondered if they, too, had dangerous levels of lead in their soil.

7. HIV diagnoses hit Georgia hard, and the feds took major action. President Trump’s administration announced an anti-HIV plan that targeted four populous metro Atlanta counties — Fulton, DeKalb, Gwinnett and Cobb — among 48 counties in the nation. A report, using data from the CDC, ranked Georgia No. 3 in HIV risk in the nation, trailing only Ohio and Nevada. Georgia has the leading rate of new diagnoses among all the states, with 30 per 100,000 people. And rural areas in Georgia also have high rates of HIV. To prevent the spread of infections, the General Assembly passed legislation to facilitate needle exchanges among intravenous drug users, a tactic once considered radical in the state.
8. Regulations changed, and transparency became the watchword. The Georgia General Assembly passed major changes to the state’s powerful, sometimes controversial health care regulatory system known as certificate of need. The changes included giving Cancer Treatment Centers of America a way to expand the capacity of its Newnan facility and treat more Georgia patients. Another bill required that nonprofit hospitals reveal more to the public about their financial activity, including reporting top salaries, property holdings and business ventures.
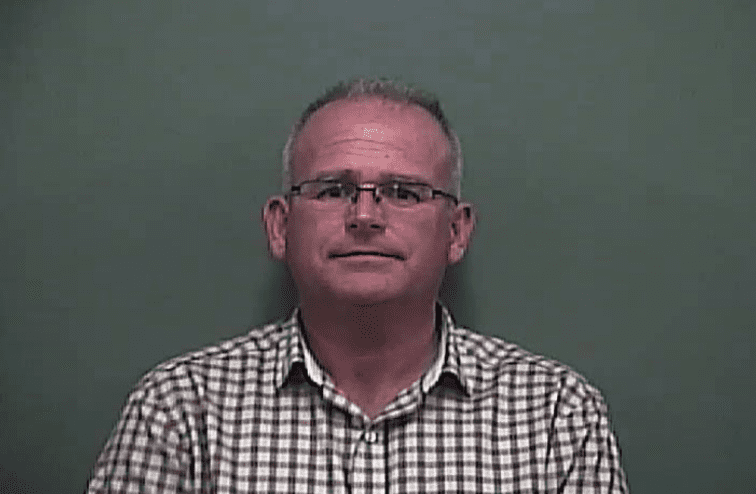
9. The state insurance commissioner was indicted. A federal grand jury accused Georgia Insurance Commissioner Jim Beck, who had been on the job just a few months, of swindling his former employer out of $2 million, in part to fund his 2018 campaign for the post. (The charges did not involve his conduct in office.) Beck denied all charges and vowed to fight them, but was suspended from his position while the case played out.
10. Consolidation reshaped the hospital business.The big just kept getting bigger throughout Georgia, and out-of-state players were heavily involved in the dealing. North Carolina-based Atrium Health announced plans to assume control of Floyd Medical Center in Rome. And in South Georgia, Tennessee-based HCA looked to expand its Georgia hospital network by entering talks to add Meadows Regional Medical Center in Vidalia. Meanwhile, in the Atlanta suburbs, a long-delayed merger between two powerhouses, Northside Hospital and Gwinnett Health System, was finalized.