This is the first in an occasional series on rural health care in Georgia. These articles are supported by a grant from the Arthur M. Blank Family Foundation.
Dr. Michael Early practices family medicine in Fort Valley. It’s in Peach County, in the farm belt of Central Georgia, and he notes that it’s “a medically underserved area.’’
After 27 years, Early is preparing to retire, and he wants to focus now on training local medical students.
He also has a broader vision beyond his retirement. “I want to continue quality health care in Peach County,” he says. “It’s a great community.”
That’s why he reached an agreement to let Mercer University School of Medicine take over his practice. “Mercer has a mission to provide health care in medically underserved areas,” Early says.
The change will expand services in Early’s practice. They will include telemedicine that will provide more access to cardiologists, pulmonologists, endocrinologists and other specialists offered at Mercer Medicine in Macon.

Early says he reached out to Mercer for help. “I know I can’t do this forever. I felt this was a perfect match.’’
The Peach County move is the latest foray into rural areas by Mercer Medicine.
A year ago, with the help of former President Jimmy Carter, who’s also a former Georgia governor, Mercer established a new primary care practice in Carter’s hometown of Plains.
Mercer will open another primary care practice in a former hospital in Clay County, in southwest Georgia on the Alabama line.
Rural areas under pressure
The university expansion comes at an important time.
From hospital finances to disease rates to provider shortages, rural areas face major challenges.
Financial problems have led seven rural Georgia hospitals to close since 2010. That’s the third-highest total among states, trailing only Texas and Tennessee. More than half of Georgia’s remaining rural hospitals are vulnerable to closure, according to a 2016 report on rural hospital strength by iVantage Health Analytics for the National Rural Health Association.
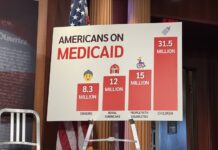
Georgia has not expanded its Medicaid program under the Affordable Care Act, and it has a high rate of people without any health coverage. Most who lack coverage are poor, and many end up unable to pay their bills at hospitals and clinics.
Rural patients tend to have more chronic disease than urban and suburban Georgians.

In addition, large areas of rural Georgia struggle with a scarcity of physicians, notably ob/gyns and pediatricians. Six of the state’s 159 counties have no physician, 63 counties are without a pediatrician, 66 without a general surgeon, and 79 without an ob/gyn, state officials say. Many parts of rural Georgia lack mental health providers as well.
The medical provider shortage is expected to deepen, a recent state report said.
State lawmakers, recognizing these deficits, have pushed some strategies to bolster rural health care. They include a stabilization fund for rural hospitals that has helped reduce hospitals’ excess costs, create mental health programs, and improve financial and other processes.
A tax credit program for rural hospital donations has brought millions of dollars to needy hospitals. The program allows a dollar-for-dollar reduction on state income taxes for those who file as individuals, couples or corporations in the state. The tax credit funding has been very successful, says state Rep. Terry England, chairman of the House Appropriations Committee.
 To fill in some physician gaps, the Medical College of Georgia is planning new incentives for med students to practice in rural areas by reducing tuition and shortening their time in school. Mercer also has such a program.
To fill in some physician gaps, the Medical College of Georgia is planning new incentives for med students to practice in rural areas by reducing tuition and shortening their time in school. Mercer also has such a program.
Mercer Medicine says its two new facilities in Peach and Clay counties will provide an educational component for rural physicians, management services and will help in the placement of future physicians.
Dr. Jean Sumner, dean of the Mercer University School of Medicine, says, “We’re committed to our mission. We’re committed to change the health status of rural Georgia.’’
Such service expansions are necessary for rural Georgia, says Jimmy Lewis, CEO of HomeTown Health, an association of rural hospitals in the state. “There have to be creative solutions,’’ he says. “One size doesn’t fit all.’’
In Plains, Mercer refurbished a clinic building before it opened last summer.
“Under President Underwood’s and Dr. Sumner’s leadership, graduates at Mercer stay in state and practice at about twice the national average, and of those who practice in Georgia, about 80 percent choose to stay in a community that’s either rural or underserved,” former President Carter said when the clinic opened. “That’s a great achievement for Mercer, and we look upon Plains as just one step toward Mercer’s even greater greatness.’’
The Plains clinic continues to expand services, adding a part-time ob/gyn and now performing X-rays. “The facility is doing great,’’ says Charles Duffey, chief operating officer of Mercer Medicine. “The community response has been overwhelming.’’
The Clay County center, which will open next year, will offer primary care, X-ray services, on-site lab services, vaccinations and telehealth providers. The Georgia county has had only one physician, Dr. Karen Kinsell, for years.

The Clay County Board of Commissioners and Development Authority will renovate the former hospital in Fort Gaines and will also provide office space for the Georgia Department of Public Health.
“Mercer Medicine brings extensive experience and expertise to our area that will develop a medical clinic in Fort Gaines to serve as a trusted source of quality care for our residents and the surrounding area,” said Clay County Administrator Ronnie Crozier in a statement.
21st century technology
Telemedicine is a big component in the Mercer Medicine work. The use of long-distance video technology not only lets physicians see patients they would not otherwise see, but it also allows medical professionals in far-flung communities to consult with one another.
If you’re a solo physician, Sumner says, “you can see incredibly complex patients. Sometimes you just want a second opinion.’’
Telemedicine can provide an ultrasound for a pregnant woman who would otherwise “have to drive 80 miles to see an ob/gyn,’’ she says.
Charles Owens, director of the Center for Public Health Practice and Research at Georgia Southern University, says the Mercer clinics will encourage economic development in many communities by improving the availability of health care in those places.

“It is exciting to see Mercer increasing health care services in rural communities by giving medical students an opportunity to learn ‘first-hand’ about the delivery of health care in a rural community,’’ Owens says. “Training providers in rural and underserved communities has proven to greatly increase the likelihood that the providers will choose communities like where they received their training.
“The Mercer clinics are a great step forward for these communities.’’
And the Macon-based university may not be finished expanding.
“Southwest Georgia needs us. Southeast Georgia needs us,’’ Sumner says. “We want to go to areas of most need.”