A new analysis underscores the enormous challenges that Georgia faces in fighting HIV.
The state ranks No. 3 in HIV risk in the U.S., trailing only Ohio and Nevada, according to the study from Health Testing Centers, which used data from the CDC. Georgia has the leading rate of new diagnoses among states, with 30 per 100,000 people. Only Washington, D.C., has a higher new diagnosis figure.
The analysis showed that seven of the 10 states with the highest HIV risk are in the South.

That’s not surprising, said Dr. Wendy Armstrong of Emory University, medical director of the Infectious Disease Program at Grady Health System. The South typically ranks as the worst region for HIV diagnoses in such reports, she said.

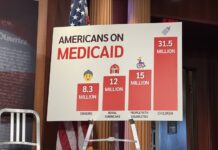
Armstrong cited factors such as a social stigma surrounding people with HIV, and the fact that several Southern states have declined to expand their Medicaid programs, which would give health coverage to more low-income people.
Other barriers in the region, she said, include poverty, lack of access to health care, lower levels of funding than other areas, and a shortage of personnel who can provide the necessary help to HIV patients.
HIV is the virus that causes AIDS, a disease that has killed millions around the world. Much progress has been made in keeping patients alive by thwarting the development of the full-scale disease, but a key to anti-HIV strategy is preventing new infections.
Among the study’s national findings:
- African-Americans are the most at risk with 49.8 per 100,000 people diagnosed with HIV. White people are the least at risk with 5.9 cases per 100,000.
- People between 25 and 34 are most likely to be diagnosed with HIV, followed by people ages 35 to 44 and 13 to 24.
- Men have a much higher risk of contracting HIV, with 23.1 cases per 100,000, while for women the number is 5.2.
- Male-to-male sexual contact accounts for 66.8 percent of HIV transmission, followed by heterosexual contact at 23.6 percent.
 Georgia was ranked No. 6 in the nation for worst AIDS death rates, with 7.2 AIDS deaths per 100,000 people, and No. 10 for lack of medical treatment with, 71.5 percent of HIV-positive individuals receiving medical treatment for HIV.
Georgia was ranked No. 6 in the nation for worst AIDS death rates, with 7.2 AIDS deaths per 100,000 people, and No. 10 for lack of medical treatment with, 71.5 percent of HIV-positive individuals receiving medical treatment for HIV.
“Georgia’s HIV, hepatitis and STI [sexually transmitted infection] rates are atrocious,’’ said Cathalene Teahan of the Georgia AIDS Coalition.
But she noted that the Georgia General Assembly passed a bill earlier this year that would facilitate needle exchange programs. Such programs allow drug users to get clean needles instead of sharing and reusing the old ones.
Another bill that was approved would establish a pilot program for distributing PrEP (pre-exposure prophylaxis), a drug used to prevent HIV. Through daily use, people at high risk of getting the virus can lower their chances of becoming infected.
“If we are going to prevent HIV transmissions, then access to clinical visits and recommended lab services are a critical component of PrEP and should be covered [by insurance] with no cost sharing,’’ Teahan said Monday.
Earlier this year, President Trump announced an anti-HIV plan that targeted four populous metro Atlanta counties — Fulton, DeKalb, Gwinnett and Cobb — among 48 counties in the nation.

Rural areas of Georgia need attention, too, Teahan said. HIV and hepatitis testing must increase, as well as housing options, especially for young people, she said. “There is a lot of focus in the Atlanta and metro areas,’’ she said. “We cannot forget our rural areas.”
Emory’s Armstrong, along with a colleague, wrote a recent paper calling for a broad effort on HIV in the South.
“We must ensure that everyone at risk and living with HIV has unfettered access to high-quality, continuous and culturally competent, stigma-free prevention and treatment services,’’ she said.
The fight should include tapping political will at the local, regional and federal levels, economic investment for direct and supportive services, and initiatives to reduce stigma in the community and the health care setting, Armstrong said.