
Low-income adults in states that haven’t expanded Medicaid are more likely to have unmet medical needs than the poor in states that expanded the government-run program, a federal report says.
The report from the Government Accountability Office (GAO), released Monday, based its estimates from a 2016 national survey. An estimated 5.6 million uninsured low-income adults had incomes eligible for expanded Medicaid as outlined under the Affordable Care Act. Most of them reside in the 17 states, including Georgia, that have not adopted expansion.
Medicaid expansion has become a campaign issue in the upcoming gubernatorial election in Georgia.
The state’s Republican political leadership has consistently rejected expansion, saying it’s too costly. Democrat Stacey Abrams has made her support of expansion a major topic in her campaign for governor, while Republican Brian Kemp opposes the move.
Expansion is also an issue in governor’s races in Florida and Wisconsin, and is on the ballot in referendums in in Idaho, Nebraska and Utah, the Associated Press noted. Montana voters will decide on maintaining that state’s expansion program.

Among the report’s findings, as summarized by the AP:
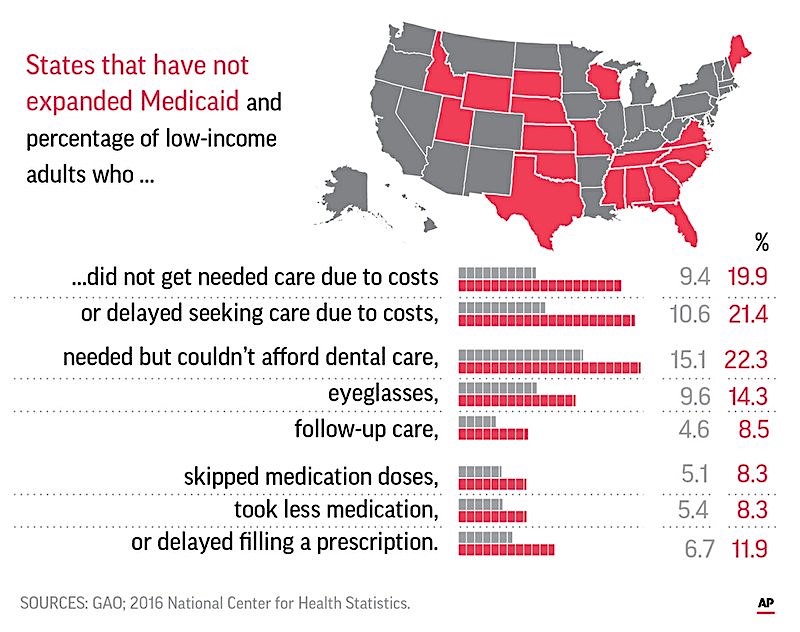
• Nearly 20 percent of low-income people in states that did not expand Medicaid said they passed up needed medical care in the past 12 months because they couldn’t afford it. That compared to 9.4 percent in states that expanded the program.
• About 8 percent of those in states that did not expand Medicaid reported they either skipped medication doses to save money or took less medication than was prescribed. That compared to about 5 percent in states that expanded Medicaid.
• About 22 percent of those in states not expanding Medicaid said they needed but could not afford dental care, as compared to 15 percent of similar poor adults in expansion states. (Medicaid provides limited dental services.)
• About 11 percent of those in non-expansion states said they needed to see a physician specialist but weren’t able to afford it, as compared to about 6 percent of those in expansion states.
David Howard, a health economist at Emory University, said the GAO study only compared access to care at a point in time and did not measure outcomes before and after Medicaid expansion.
“Still, the results are consistent with what we know from better-designed studies, such as the Oregon Experiment, where a lottery was used to determine Medicaid eligibility,’’ Howard said Monday. “Low-income people who get Medicaid use more care and are less likely to report that they went without needed care.”

Oregon held a lottery for uninsured adults to gain Medicaid coverage in 2008. Later, research compared lottery winners to those who didn’t receive coverage.
The studies found gaining Medicaid in Oregon was associated with higher rates of health care use, a lower probability of having medical debts sent to a collection agency, and higher self-reported mental and physical health. Researchers also found that Medicaid increased emergency department visits.
About two years after the lottery, studies found that Medicaid increased use of health care services, raised rates of diabetes detection and management, lowered rates of depression, and reduced financial strain.

Seema Verma, administrator of the Centers for Medicare and Medicaid Services, says Medicaid was originally intended as a safety-net program for the most vulnerable in society and covering able-bodied adults is beyond its scope, the AP said. Verma is encouraging states to set work requirements for Medicaid, saying that step will encourage people to earn their way out of poverty and dependence on government insurance.
Supporters of Medicaid expansion say the argument for it is growing stronger.
“It’s the same as we’ve seen more broadly with the ACA,” Judy Solomon of the Center on Budget and Policy Priorities, which advocates for low-income people, told the AP. “It’s here to stay, and states that haven’t been able to get it over the finish line are questioning themselves.”







