This year, a COVID-19 pandemic policy that kept millions of people covered by Medicaid without interruption came to an end. Continuous enrollment protected adults and children from losing their healthcare coverage even if they were no longer eligible.
But now, many people are at risk of losing their Medicaid coverage, especially if they don’t know what to do. And advocates say some outreach efforts from state public health departments have not been effective in reaching vulnerable communities.
That’s why at a festival in downtown Byromville, Kristen Kiefer talked to people about Medicaid Unwinding, which is another term for the redetermination process which began April 1.
“Medicaid has started doing renewals again this year,” Kiefer said. “And we’re running into a lot of people that don’t know that the renewals have started again.”
Kiefer is with the American Cancer Society Cancer Action Network (ACS CAN), a non-government nonprofit trying to spread awareness about Medicaid Unwinding.
Normally, people receiving benefits through Medicaid or PeachCare for Kids have their eligibility checked annually. But states across the country started redeterminations again this year as part of a federal mandate.
April 1 marked the first time in three years that Georgia started checking people’s eligibility under Medicaid and PeachCare for Kids. Almost 3 million people in Georgia will go through redeterminations over the next year.

That’s all news to Rosa Caldwell in Byromville, who said she knows several people on Medicaid.
“I know my husband, I need to do his. He’s 69; he needs to renew his,” Caldwell told Kiefer. “And I was looking for my sister-in-law and my brother — he just turned 68 — they both get Medicaid.”
Kiefer said so far, she’s encountered a lot of confusion about Medicaid Unwinding. So everyone who comes up to Kiefer at events like this gets a pamphlet with important dates and information, and she encourages them to tell their friends and family.
“We don’t want anybody to miss their date because they didn’t realize that it was coming,” Kiefer said.
State officials are relying on groups like ACS CAN to get the word out and report back with feedback on outreach efforts. Like official state ads on Facebook that tell people to “stay covered.” The ads are cute. There’s a mascot, a peach with googly eyes named George A. Peach. It’s part of the state’s marketing strategy.
But when Kiefer monitors the thousands of comments on these ads, she gets concerned. Some comments point to people not understanding whether the redetermination process applies to them or not. Other comments lead Kiefer to believe that people think redeterminations are a scam.
There are hardly any comments from public health officials to clear things up.
“The kind of lack of public information or confusion around this issue leads to well-meaning people kind of misinforming them in reply to their comment seeking help,” Kiefer said. “And it’s just been kind of a challenge.”
Heather Howard, health care policy expert from Princeton University, says confusion about Medicaid Unwinding is “exactly what we predicted.”
“One thing we’ve learned is that you have to make it really simple; people do not understand,” Howard said about messaging.
That’s because, for a long time, people haven’t had to think about their Medicaid coverage and how to make sure they don’t lose it.
Different outcomes for different groups
So how is Georgia going about all of this?
People going through Medicaid redeterminations are put in two different buckets, said the state’s executive director for Medical Assistance Plans, Lynnette Rhodes, during a meeting of the Care Management Committee in May.
“Bucket A are those individuals who are auto-renewed,” Rhodes said. “The member doesn’t have to do or take any action.”
Bucket A people will stay on Medicaid until renewals next year.
“Bucket B are those individuals who cannot be auto-renewed,” Rhodes said.
People in Bucket B have missing information about their eligibility that the state needs. These are the people who might accidentally lose coverage.
According to data from the Georgia Department of Community Health, 12,526 people received renewal notices in May.
By the end of the month, 1,581 of those people had their Medicaid coverage terminated due to procedural reasons, meaning they didn’t respond to notices or turn in missing information.
Georgia’s unwinding plan makes it so that anyone terminated from Medicaid for procedural reasons has 90 days to prove they are still eligible.
State officials plan that in June, 227,000 people will go through redeterminations.
Unclear communication
The only way for people to know which bucket they’re in and what to do to keep Medicaid coverage is to check the same online portal the state uses for most social services, called Georgia Gateway. That’s where people’s renewal dates and notices are posted.
The unwinding ads on Facebook don’t make that clear. Fliers from the state aren’t clear enough either, said the director at First Choice Primary Care, Katherine McLeod.
“I mean, this doesn’t say, ‘Get help,’ right?” McLeod said. “This just says, ‘Hey, something’s happening.’”
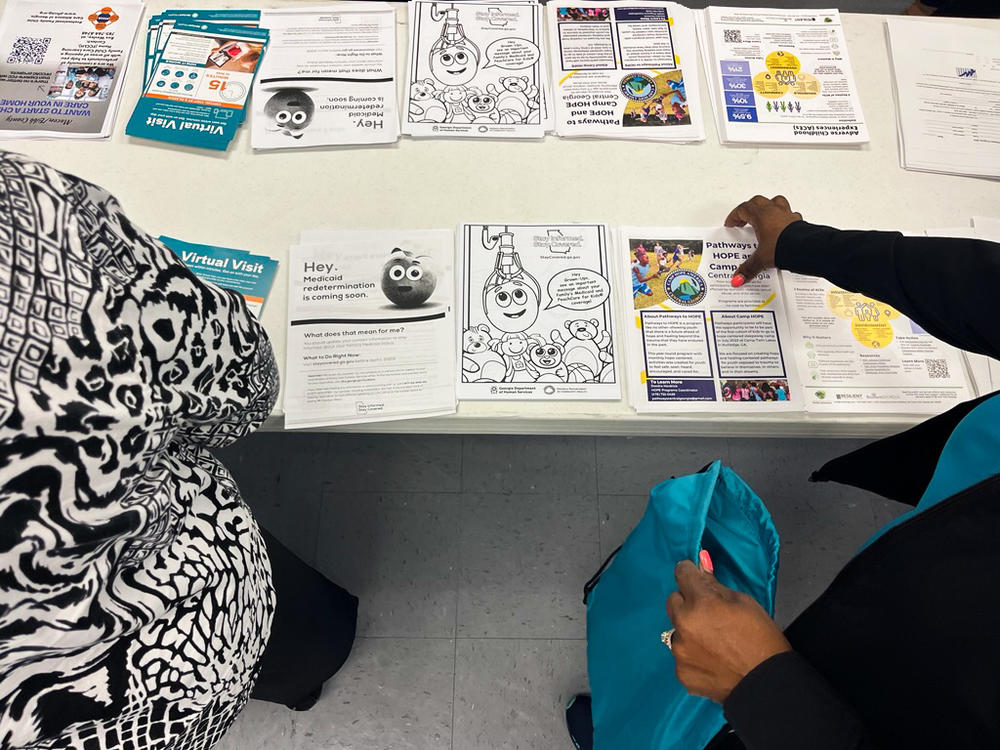
The fliers come from Georgia’s “Stay Covered” website, the online hub for the state’s information on Medicaid Unwinding. There are materials posted in a variety of languages and a coloring sheet for kids featuring the George A. Peach character.
The state wants its fliers posted in healthcare settings like First Choice in Macon. About a quarter of patients at First Choice are insured through Medicaid, McLeod said.
But Felicia Cornelius, outreach director at First Choice, said the information on the flier isn’t patient-friendly enough.
“If you have a normal person that is reading this, I don’t think it really still helps them to be able to figure out, ‘OK, what do I need to do?’” Cornelius said. “I think it’s more partner than consumer.”
But what if partners still have questions?
Cornelius said the handful of patients she’s helped renew their Medicaid coverage are homeless. Weeks ago, she asked state officials about a plan for how her homeless patients can receive notices about renewals. Cornelius said she hasn’t seen a plan yet.
Meanwhile, it’s possible many of the over 1,500 people who lost their Medicaid coverage last month did so without knowing why.
Looking forward, policy analysts warn that coverage losses overall are more likely in states without Medicaid expansion, like Georgia, because even slight changes in income can make people ineligible for coverage. Unlike expansion states which offer Medicaid up to 138% of the federal poverty level, Medicaid in Georgia is capped at 100% of the FPL for most people.
__________
This article comes to Now Habersham through a partnership with GPB News